Cataract Treatment in Vileparle and Santacruz
Cataract Diagnosis & Treatment


Best Neuro Ophthalmologist in Mumbai
What is Neuro Ophthalmology?
Neuro Ophthalmology Symptom Checker
- Blurred vision/ Visual loss
- Visual field defects of sudden onset or progressive.
- Double vision of sudden onset.
- Disorders of eye movement of sudden onset.
- Sudden onset of drooping of eyelids.
-
Headache due to migraine, stress, cluster
headache and closely related conditions. - Transient visual loss.
- Facial paralysis.
- Abnormal involuntary movements of the eyes and face.
Causes of Glaucoma
- Build-up of aqueous humor inside the eye
- Genetic reasons
- Birth defects
- Blunt or chemical injury
- Acute eye infection
- Blockage by blood vessels inside the eye
- Inflammatory conditions
- In rare cases, previous eye surgeries
Types of Glaucoma
The most prevalent form of glaucoma is known as primary open-angle glaucoma. In this type, the drainage passage for the fluid within the eye remains open, allowing fluid outflow. However, there may be a flaw in the drainage pathway, resulting in increased resistance to fluid drainage, leading to heightened eye pressure. In a small percentage of cases, increased fluid production can also contribute to the elevated pressure. This type of glaucoma develops slowly and does not initially present any symptoms. It first affects the side vision, gradually progressing towards the center of vision. Due to this gradual progression, many individuals may remain unaware of their condition until they experience significant vision loss that affects their central vision.
Risk factors for primary open angle glaucoma are:
- Age more than 40 years
- Race – African Americans
- Family history of glaucoma
- Systemic diseases such as diabetes mellitus, hypertension, heart disease
- High myopia or those with a high minus power
Angle closure glaucoma, also known as closed angle glaucoma, is the second most common type of glaucoma and is characterized by narrow drainage channels in the eye. If the angle gradually closes over time, it is referred to as chronic angle closure, while a sudden closure of the angle leads to an acute angle closure attack. Acute angle closure glaucoma presents as a medical emergency. During an acute attack, the patient experiences symptoms such as eye pain, nausea, vomiting, redness, blurred vision, and colored halos due to a rapid increase in eye pressure. Immediate treatment by an eye specialist is essential in such cases.
Risk factors for angle closure glaucoma:
- Age more than 40 years
- Race – East Asians
- Family history of glaucoma
- Women
- High hypermetropia or those with a high plus power
Normal tension glaucoma, also referred to as low tension glaucoma, is a type of glaucoma where damage to the optic nerve can occur despite the eye pressure being within the normal range. The exact cause of this condition is not fully understood, but it is believed to stem from either an exceptionally delicate optic nerve that can be harmed even with normal eye pressure or reduced blood flow to the optic nerve. This type of glaucoma is often asymptomatic, and individuals typically do not experience any visual complaints until the disease reaches a very advanced stage.
Risk factors for normal tension glaucoma are:
- Family history of normal tension glaucoma
- Race – Japanese ancestry
- Thinner corneas
- Heart disease
- Migraine and peripheral vascular disease
Glaucoma during infancy and childhood is a relatively uncommon but serious set of diseases that can jeopardize vision. Infants and young children with glaucoma are usually brought for an eye examination because either their parents or pediatricians have observed some peculiarities in their eyes. These signs may include whitish discoloration and enlargement of the eyes, excessive tearing, a tendency to keep the eyes closed, and sensitivity to light. Glaucoma in children may arise if there’s a family history of glaucoma, if the parents have had a consanguineous (close blood relation) marriage, or due to abnormal development during pregnancy.
This type of glaucoma occurs due to an irregular flow of intraocular fluid within the eye caused by a blockage or dysfunction of the trabecular meshwork, which are the drainage canals in the eye with a mesh-like structure. Alternatively, in certain instances, the abnormal drainage system can be a consequence of another eye or body condition, leading to what is known as secondary glaucoma.
Congenital glaucoma is identified through a comprehensive eye examination, typically conducted under sedation in the operating theater for infants and children below the age of 3. Early detection and treatment of congenital glaucoma can help slow down the progression of the condition. Microsurgery is often used to address structural defects in straightforward cases of congenital glaucoma. For more complex cases, a combination of medication and surgery is employed for treatment.
Secondary glaucoma refers to specific types of glaucoma in which the underlying reason for increased eye pressure leading to optic nerve damage and vision loss can be identified. Various factors contribute to secondary glaucoma, such as the prolonged and unregulated use of steroids, severe diabetic retinopathy, eye injuries, inflammation of the eye (uveitis), or advanced stages of cataract.
If you suspect having any of these risk factors, it is important to undergo an eye examination. Remember to inform your eye doctor about your specific risk factors, which will assist them in determining the frequency of your eye check-ups. The type of treatment prescribed will be based on whether you have open-angle or angle-closure glaucoma.
Secondary open-angle glaucoma can be a result of eye injury. Traumatic glaucoma can manifest immediately after the injury or emerge years later. It can be triggered by blunt trauma, which bruises the eye, or by penetrating injuries. In most cases of blunt trauma, the elevated eye pressure is temporary. However, there are instances where the drainage canals in the eye sustain damage and permanent scarring occurs. This scarring obstructs fluid flow and may lead to glaucoma even years after the initial injury.
Furthermore, conditions like myopia (nearsightedness), previous eye injury, infections, or past surgeries can increase the susceptibility of the eye to severe injuries.
Pseudoexfoliative Glaucoma, a type of secondary open-angle glaucoma, occurs when a flaky material similar to dandruff peels off from the outer layer of the eye’s lens. This material accumulates in the angle between the cornea and iris, potentially blocking the eye’s drainage system and leading to increased eye pressure. Pseudoexfoliative Glaucoma is frequently observed in individuals of Scandinavian descent.
Individuals diagnosed with exfoliative glaucoma commonly experience more instances of elevated eye pressure, greater fluctuations in pressure, and higher peak pressures compared to patients with other forms of glaucoma. Managing this type of glaucoma with medical treatment alone is typically more challenging. Patients with exfoliative glaucoma necessitate aggressive medical therapy and are more likely to require laser or surgical interventions. Regular and frequent visits to their eye doctor are often essential to closely monitor the progression of the disease.
A type of secondary open-angle glaucoma can be triggered by the atypical growth of new blood vessels on the iris and across the eye’s drainage channels.
Neovascular glaucoma is invariably linked to other conditions, most commonly diabetes and hypertension. It never develops in isolation. The emergence of new blood vessels obstructs the normal drainage of eye fluid through the trabecular meshwork, resulting in elevated eye pressure. This type of glaucoma advances swiftly and poses significant challenges in terms of treatment.
Glaucoma Risk Factors
You are most likely to get glaucoma if you:
- Are you over 60 years of age
- Have high internal eye pressure
- Have a family member diagnosed with glaucoma
- Have certain conditions like diabetes, heart conditions, sickle cell anaemia and high blood pressure.
- Have thin corneas
- Have extreme conditions of nearsightedness or farsightedness
- Have had eye injuries, surgeries
- Taking corticosteroid medications for a long time
Glaucoma Technology

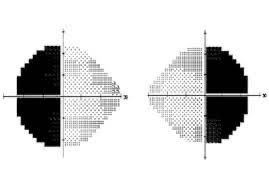
Zeiss Humphrey Field Analyzer 3
- Visual Field Testing for the purposes of screening, monitoring, and assisting in the diagnosis and management of ocular diseases such as glaucoma and related neurological disorders.
- Easy to perform
- Extremely repeatable
- Progression mapping :- Provides information about stability/progression of disease

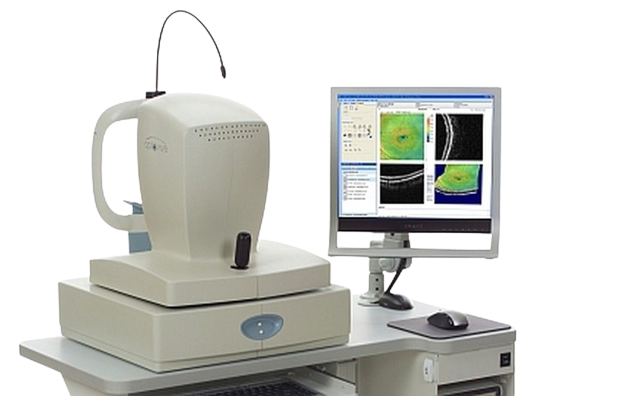
OPTOPOL Revo FC OPTICAL COHERENCE TOMOGRAPHY(OCT)
- OCT ONH (Glaucoma) helps in precise diagnosis and monitoring of glaucoma progression over time
- Pachymetry and Epithelial Thickness help in Refractive Surgery Assessment as well in detection of Corneal Ectatic Conditions like Keratoconus

Optovue RTVue OPTICAL COHERENCE TOMOGRAPHY
- Gold Standard in Epithelial mapping due to second to none accuracy and precision
- OCT ONH (Glaucoma) helps in precise diagnosis and monitoring of glaucoma progression over time
- Pachymetry and Epithelial Thickness help in Refractive Surgery Assessment as well in detection of Corneal Ectatic Conditions like Keratoconus
Zeiss Humphrey Field Analyzer 3
OPTOPOL Revo FC OPTICAL COHERENCE TOMOGRAPHY(OCT)
Optovue RTVue OPTICAL COHERENCE TOMOGRAPHY


- Visual Field Testing for the purposes of screening, monitoring, and assisting in the diagnosis and management of ocular diseases such as glaucoma and related neurological disorders.
- Easy to perform
- Extremely repeatable
- Progression mapping :- Provides information about stability/progression of disease
- OCT ONH (Glaucoma) helps in precise diagnosis and monitoring of glaucoma progression over time
- Pachymetry and Epithelial Thickness help in Refractive Surgery Assessment as well in detection of Corneal Ectatic Conditions like Keratoconus
- Gold Standard in Epithelial mapping due to second to none accuracy and precision
- OCT ONH (Glaucoma) helps in precise diagnosis and monitoring of glaucoma progression over time
- Pachymetry and Epithelial Thickness help in Refractive Surgery Assessment as well in detection of Corneal Ectatic Conditions like Keratoconus
Glaucoma Diagnosis
Regular eye examinations are crucial for maintaining eye health. At the age of 40, it is recommended to undergo a baseline eye screening to detect any early signs of eye disease or vision changes that may begin to emerge. Based on the results of this screening, your eye doctor will advise you on the frequency of follow-up exams to ensure optimal eye care.
If you possess risk factors for glaucoma, such as diabetes, hypertension, or a family history of the condition, it is advisable to schedule an appointment with an eye doctor promptly. They can assess your situation and recommend the appropriate frequency for your eye examinations.
A thorough glaucoma assessment involves a series of tests that aid in detecting the existence of glaucoma and monitoring its progression during subsequent follow-ups.
- Tonometry
- Gonioscopy
- Ophthalmoscopy
- Pachymetry
- Optic Nerve Head Oct
- The Visual Field test (Perimetry)
 Tonometry is a diagnostic procedure utilized to gauge the intraocular pressure (IOP), which is the fluid pressure inside the eye. This test holds significance as it aids the doctor in assessing the potential risk of glaucoma. For individuals already diagnosed with glaucoma, tonometry is crucial in understanding the risk of disease progression and determining the effectiveness of treatment.
Tonometry is a diagnostic procedure utilized to gauge the intraocular pressure (IOP), which is the fluid pressure inside the eye. This test holds significance as it aids the doctor in assessing the potential risk of glaucoma. For individuals already diagnosed with glaucoma, tonometry is crucial in understanding the risk of disease progression and determining the effectiveness of treatment.  Gonioscopy is a painless examination of the anterior chamber of your eye, which allows the doctor to determine whether the drainage angle, where fluid exits the eye, is open or closed. This test is vital as it enables your doctor to diagnose glaucoma accurately and customize the most suitable treatment plan for your condition.
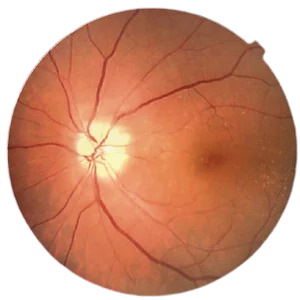
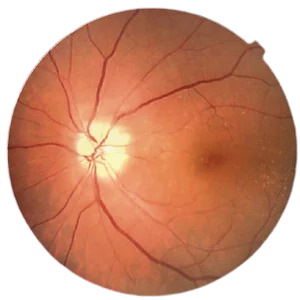
Gonioscopy is a painless examination of the anterior chamber of your eye, which allows the doctor to determine whether the drainage angle, where fluid exits the eye, is open or closed. This test is vital as it enables your doctor to diagnose glaucoma accurately and customize the most suitable treatment plan for your condition. 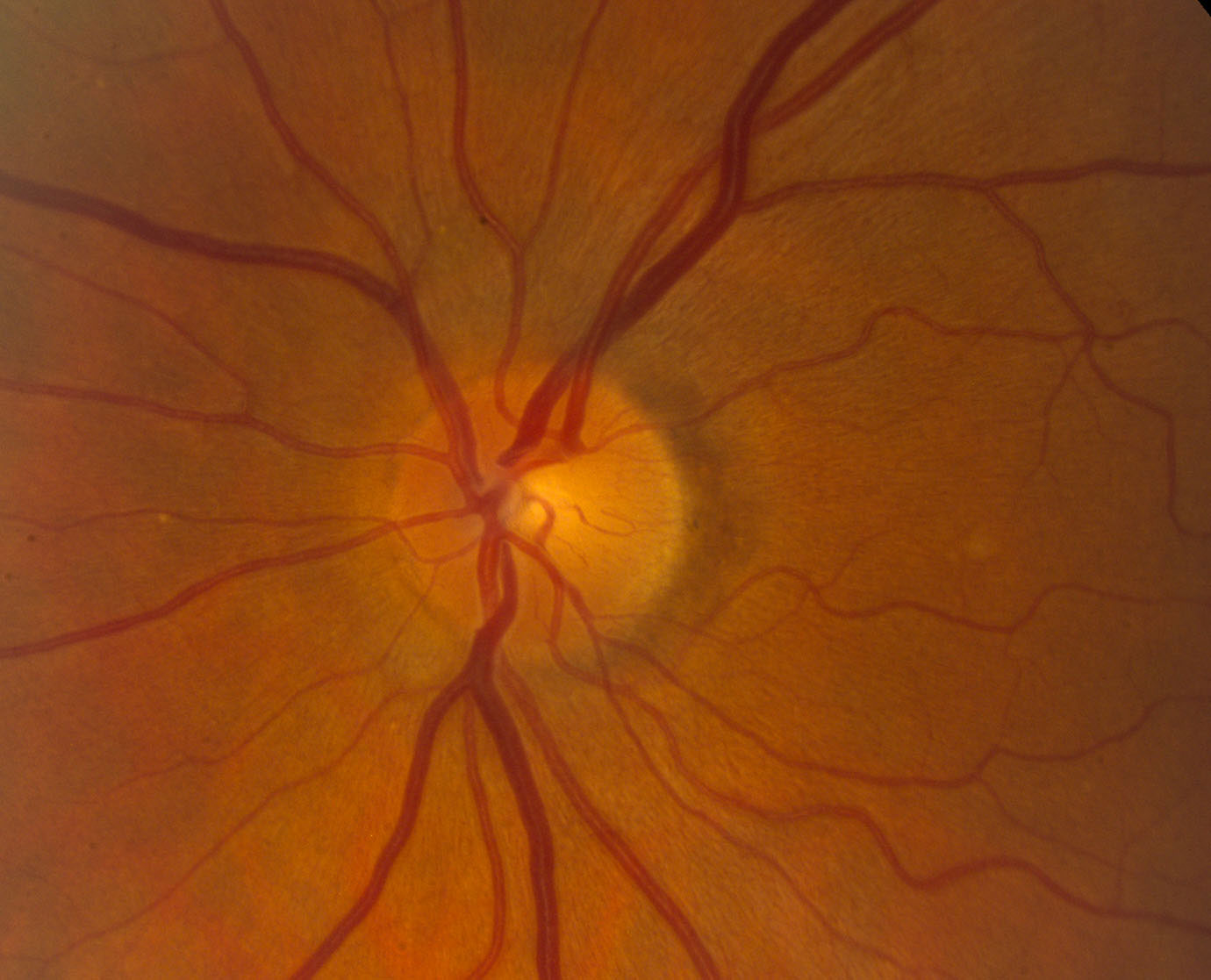 This diagnostic procedure allows the doctor to assess the damage to your optic nerve caused by glaucoma. By using eye drops to dilate the pupil, the doctor can obtain a clear view of the optic nerve, examining its shape and color through your eye.
This diagnostic procedure allows the doctor to assess the damage to your optic nerve caused by glaucoma. By using eye drops to dilate the pupil, the doctor can obtain a clear view of the optic nerve, examining its shape and color through your eye.  This diagnostic method assists in assessing the thickness of the cornea, a crucial factor in determining the Corrected IOP (Intraocular Pressure).
This diagnostic method assists in assessing the thickness of the cornea, a crucial factor in determining the Corrected IOP (Intraocular Pressure).
 This method aids in the assessment of initial glaucomatous alterations on the Optic Nerve head. It provides information about the thinning of the Retinal Nerve Fiber Layer (RNFL) in different quadrants and changes in the Ganglion Cell Layer (GCC).
This method aids in the assessment of initial glaucomatous alterations on the Optic Nerve head. It provides information about the thinning of the Retinal Nerve Fiber Layer (RNFL) in different quadrants and changes in the Ganglion Cell Layer (GCC).
The Perimetry, also known as the Visual Field test, creates a comprehensive map of your entire field of vision. By examining your peripheral or side vision, which is usually impacted first by glaucoma, your doctor can diagnose and track the progression of the condition. The test results are crucial in assessing the severity of glaucoma, the extent of vision loss, as well as any damage to the visual pathways in the brain and other optic nerve-related disorders.
Once a thorough evaluation of the patients is completed, doctors engage in discussions regarding the most suitable treatment options available. These options may include topical eye drops, oral medications, or interventional procedures such as lasers or surgeries. Patients are encouraged to inquire and express any concerns they may have, and doctors make an effort to address all their queries with care and attentiveness.
The utilization of these novel investigative techniques enables us to identify the disease and its progression at an earlier stage, leading to improved patient management.
NEURO OPHTHALMOLOGY CONDITIONS
Optic Neuropathies
Conditions impacting the optic nerve, such as optic neuritis, ischemic optic neuropathy, autoimmune optic neuropathy, compressive optic neuropathy, nutritional optic neuropathy, and toxic optic neuropathy.
Demyelination Disorders
Disorders involving demyelination that impact the visual pathway comprised of the optic nerve, optic chiasma, optic tract, and optic radiations.
Other Conditions Causing Raised Intracranial Pressure
Additional factors inducing heightened pressure within the skull, such as idiopathic intracranial hypertension and cerebral venous thrombosis, may lead to enduring and significant visual impairment over an extended period.
Ocular Motility Disorders
Ocular movement disorders marked by partial or total incapacity to control the movement of one or both eyes, stemming from diseases affecting the central and peripheral nervous systems, such as myasthenia gravis, or ocular motor cranial nerve impairments arising from factors like trauma, tumors, or systemic conditions like hypertension or diabetes mellitus.
Tumours
Tumors such as pituitary adenoma, craniopharyngioma, and meningioma leading to compressive optic neuropathy by exerting direct pressure on the optic nerve, along with other brain tumors that impact the visual pathway and contribute to increased intracranial pressure.
Cerebrovascular Disorders
Cerebrovascular conditions causing vision loss, transient ischemic episodes resulting in momentary visual impairment.
Neuro Ophthalmology Diagnosis
- Fundus Photography
- Visual Field Test (Perimetry)
- OCT Optic Nerve Head
- MRI / CT Scan Brain
Neuro Ophthalmology Diagnosis
- Fundus Photography
- Visual Field Test (Perimetry)
- OCT Optic Nerve Head
- MRI / CT Scan Brain
Neuro Ophthalmology Diagnosis
- Fundus Photography
- Gonioscopy
- Ophthalmoscopy
- Pachymetry
- Optic Nerve Head Oct
- The Visual Field test (Perimetry)
- The Visual Field test (Perimetry)
 Tonometry is a diagnostic procedure utilized to gauge the intraocular pressure (IOP), which is the fluid pressure inside the eye. This test holds significance as it aids the doctor in assessing the potential risk of glaucoma. For individuals already diagnosed with glaucoma, tonometry is crucial in understanding the risk of disease progression and determining the effectiveness of treatment.
Tonometry is a diagnostic procedure utilized to gauge the intraocular pressure (IOP), which is the fluid pressure inside the eye. This test holds significance as it aids the doctor in assessing the potential risk of glaucoma. For individuals already diagnosed with glaucoma, tonometry is crucial in understanding the risk of disease progression and determining the effectiveness of treatment.  Gonioscopy is a painless examination of the anterior chamber of your eye, which allows the doctor to determine whether the drainage angle, where fluid exits the eye, is open or closed. This test is vital as it enables your doctor to diagnose glaucoma accurately and customize the most suitable treatment plan for your condition.
Gonioscopy is a painless examination of the anterior chamber of your eye, which allows the doctor to determine whether the drainage angle, where fluid exits the eye, is open or closed. This test is vital as it enables your doctor to diagnose glaucoma accurately and customize the most suitable treatment plan for your condition. 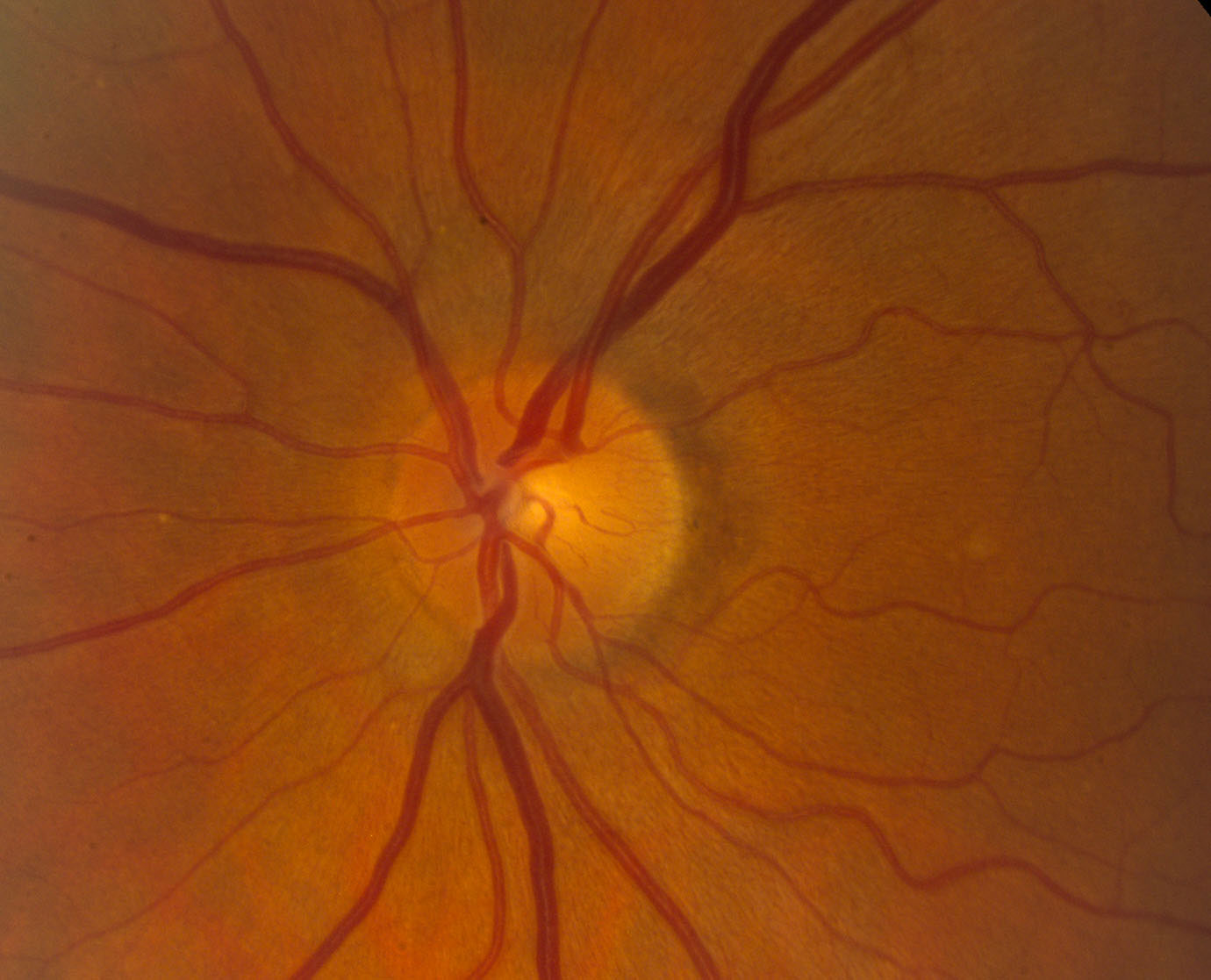 This diagnostic procedure allows the doctor to assess the damage to your optic nerve caused by glaucoma. By using eye drops to dilate the pupil, the doctor can obtain a clear view of the optic nerve, examining its shape and color through your eye.
This diagnostic procedure allows the doctor to assess the damage to your optic nerve caused by glaucoma. By using eye drops to dilate the pupil, the doctor can obtain a clear view of the optic nerve, examining its shape and color through your eye.  This diagnostic method assists in assessing the thickness of the cornea, a crucial factor in determining the Corrected IOP (Intraocular Pressure).
This diagnostic method assists in assessing the thickness of the cornea, a crucial factor in determining the Corrected IOP (Intraocular Pressure).
 This method aids in the assessment of initial glaucomatous alterations on the Optic Nerve head. It provides information about the thinning of the Retinal Nerve Fiber Layer (RNFL) in different quadrants and changes in the Ganglion Cell Layer (GCC).
This method aids in the assessment of initial glaucomatous alterations on the Optic Nerve head. It provides information about the thinning of the Retinal Nerve Fiber Layer (RNFL) in different quadrants and changes in the Ganglion Cell Layer (GCC).
The Perimetry, also known as the Visual Field test, creates a comprehensive map of your entire field of vision. By examining your peripheral or side vision, which is usually impacted first by glaucoma, your doctor can diagnose and track the progression of the condition. The test results are crucial in assessing the severity of glaucoma, the extent of vision loss, as well as any damage to the visual pathways in the brain and other optic nerve-related disorders.
 The Perimetry, also known as the Visual Field test, creates a comprehensive map of your entire field of vision. By examining your peripheral or side vision, which is usually impacted first by glaucoma, your doctor can diagnose and track the progression of the condition. The test results are crucial in assessing the severity of glaucoma, the extent of vision loss, as well as any damage to the visual pathways in the brain and other optic nerve-related disorders.
The Perimetry, also known as the Visual Field test, creates a comprehensive map of your entire field of vision. By examining your peripheral or side vision, which is usually impacted first by glaucoma, your doctor can diagnose and track the progression of the condition. The test results are crucial in assessing the severity of glaucoma, the extent of vision loss, as well as any damage to the visual pathways in the brain and other optic nerve-related disorders. 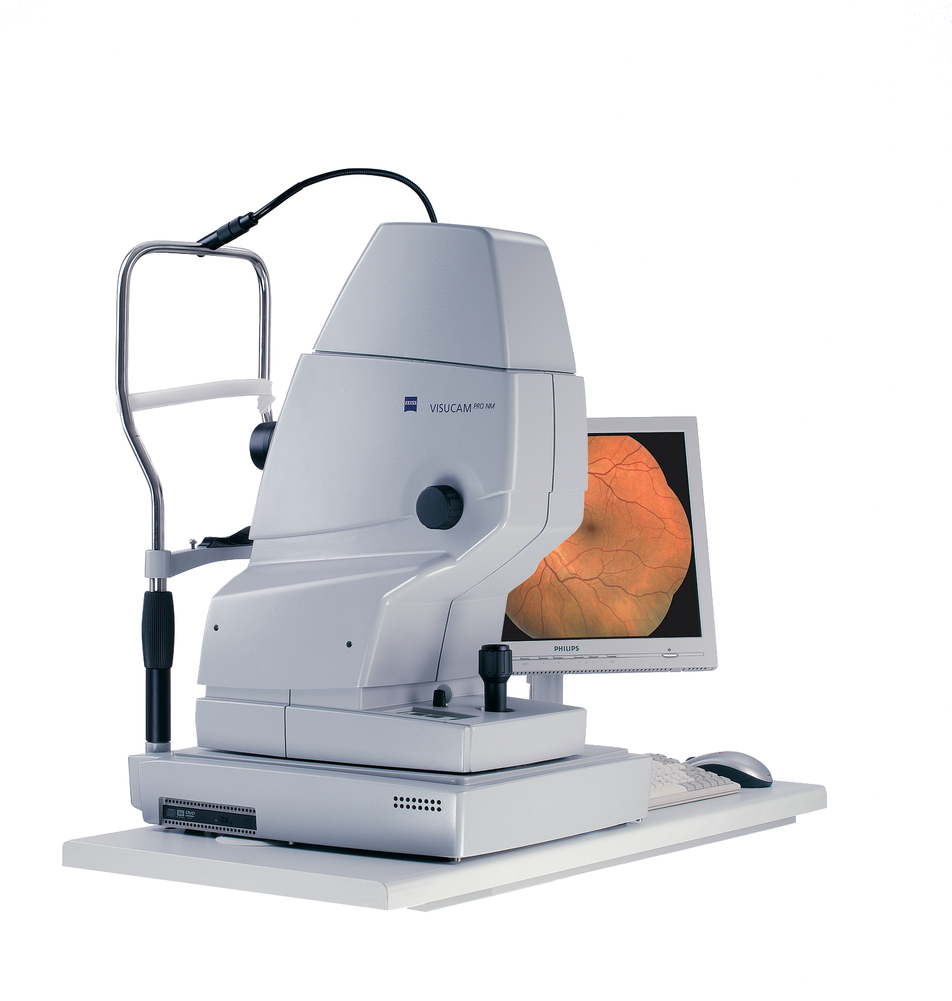
Fundus Photography
Neuro Ophthalmology Doctors

Dr. Nitin
Balakrishnan
Cataract & Refractive Surgeon

Dr. Nikhil Nitin Balakrishnan
Dr. Pavitra Patel Balakrishnan
Neuro Ophthalmology Reviews
Karan Kothari
Tan
Sakshi Shetty
Frequently Asked Questions
- Automated visual field assessment
- Visual Evoked Potentials (VEP) evaluation
- Optical Coherence Tomography (OCT) imaging
- Doppler scans for Carotid and Vertebral arteries
- Computed Tomography (CT) scans of the brain and eye socket
- Magnetic Resonance Imaging (MRI) scans of the brain and eye socket
- Magnetic Resonance Angiography (MRA) of brain and neck vessels
- Magnetic Resonance Venography (MRV) of the brain
- CT angiography of the brain and neck vessels
- Blood tests when deemed essential