Cataract Treatment in Vileparle and Santacruz
Cataract Diagnosis & Treatment
Retinopathy of Prematurity
Risk factors for developing Retinopathy of Prematurity (ROP)
Apart from premature birth and low birth weight, numerous other factors can elevate the vulnerability of these infants to ROP. These encompass extended oxygen usage (for lung function), sepsis (blood infection), blood transfusion, jaundice, inadequate weight gain, reduced platelet count, anemia (low hemoglobin), and intraventricular hemorrhage (brain bleeding), among others.
If your baby was born prematurely, you might be worried about ROP impacting their eyesight. Narayana Nethralaya advises an ROP assessment a few weeks after birth (initial screening before 30 days or sooner) for premature infants and those weighing under 2 kgs at birth, before hospital discharge. Early detection and prompt treatment can enhance the likelihood of maintaining vision.
Signs and Symptoms of Retinopathy of Prematurity (ROP)
Stages of Retinopathy of Prematurity (ROP)
Stages of Retinopathy of Prematurity (ROP)
Retinopathy of Prematurity (ROP) Screening
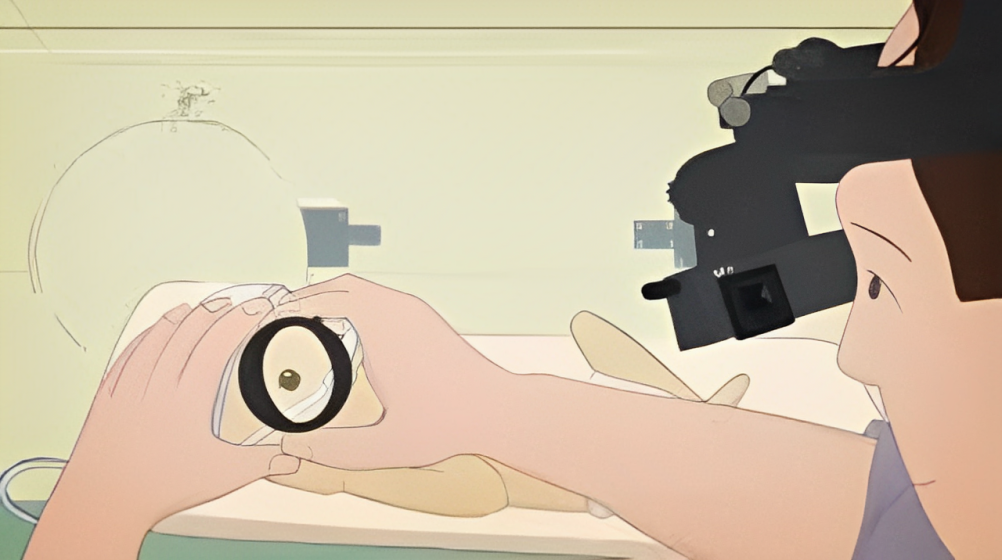
Continuous monitoring for ROP is necessary for every premature baby, extending beyond hospital discharge due to the condition’s potential delayed onset. Our team employs specialized imaging devices to conduct screenings either in the NICU of the maternity hospital or at our facility if the baby has been discharged. Should any indications of ROP become apparent, our team of experts in ROP will arrange subsequent assessments to track the baby’s progress and ascertain the appropriate timing for intervention.
Diagnosis of Retinopathy of Prematurity (ROP)

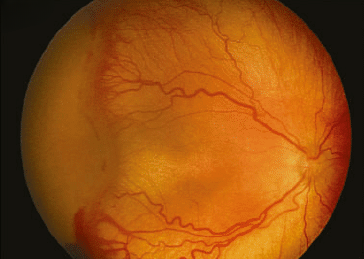
Diagnosing ROP requires the expertise of an ophthalmologist skilled in managing this condition. At Sai Deep Eye Cilinic Pediatric Retina division, advanced technology is available to identify ROP in premature infants. Our ophthalmologists possess the necessary training to diagnose ROP and will meticulously assess the retina of your preterm baby for any irregularities. This examination, which is painless and brief, typically takes only a few minutes.
Diagnosis of Retinopathy of Prematurity (ROP)
Diagnosing ROP requires the expertise of an ophthalmologist skilled in managing this condition. At Narayana Nethralaya’s Pediatric Retina division, advanced technology is available to identify ROP in premature infants. Our ophthalmologists possess the necessary training to diagnose ROP and will meticulously assess the retina of your preterm baby for any irregularities. This examination, which is painless and brief, typically takes only a few minutes.
Treatment of Retinopathy of Prematurity (ROP)
Commonly, ROP treatment employs a specialized ROP laser performed by a specialist. This procedure is conducted under topical anesthesia (via eye drops), targeting the retinal area lacking blood supply. This laser treatment yields positive results in about 90% of cases, leading to the disappearance of ROP and the preservation of eyesight. In specific scenarios, injections of a corrective drug directly into the eye (intravitreal) to counter abnormal vessel growth are also utilized. It’s noteworthy that several recipients of injections might later require laser treatment.
For advanced stages like 4 and 5 of ROP, retinal surgery is necessary. This procedure, performed under general anesthesia, is coupled with NICU support.
Failure to administer timely treatment can lead to permanent blindness or profound visual impairment in both eyes for the child. In certain cases, ROP that initially presents as Stage 1 or 2 can progress to the more severe Stage 3 or beyond. Unfortunately, the outcomes following treatment for Stage 5 ROP, even after undergoing surgery, are notably unsatisfactory.
Treatment
Vitrectomy surgery is an effective treatment for age-related macular holes at stage 2 and beyond. In this procedure, the vitreous gel inside the eye is removed, the hole is closed, and the eye is filled with a gas bubble. The gas bubble self-absorbs over a period of 4-6 weeks.
Following the surgery, certain surgeons might suggest adopting a face-down position for the first few days to expedite the hole’s closure. Stage 1 macular holes do not require surgery but necessitate regular check-ups to monitor any progression to subsequent stages. If a macular hole develops in the other eye (contralateral eye), more frequent check-ups for the unaffected eye may be recommended. Macular holes resulting from other causes generally have a less favorable outlook.

Frequently Asked Questions
The majority of ROP instances do not lead to blindness. When diagnosed promptly and if those needing treatment are identified and addressed in a timely manner, more than 90-95% of infants have favorable outcomes. The outcomes of APROP are less predictable and hinge on various factors. Unfortunately, the outcomes following treatment for Stage 5 ROP are significantly unfavorable, even after undergoing surgical intervention.
Stage 4 is characterized by an elevation of the barrier, causing the detachment of the retina from its usual position. This detachment initially occurs at the periphery of the retina and subsequently in the central visual area known as the macula. Stage 5 materializes when the retina becomes completely detached. An additional severe form of ROP known as ‘Aggressive Posterior ROP’ (APROP) bypasses stages 1 to 3 and directly enters stages 4 and 5. Diagnosing and treating APROP are especially challenging due to their distinct nature.






