Cataract Treatment in Vileparle and Santacruz
Cataract Diagnosis & Treatment
Cataract Treatment in Vileparle and Santacruz
Cataract Diagnosis & Treatment
Rhegmatogenous Retinal Detachment
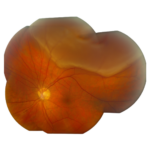
What is Rhegmatogenous Retinal Detachment?
Rhegmatogenous retinal detachment is distinguished by a retinal breach, which allows fluid to pass through and raise the neurosensory retina away from the retinal pigment epithelium. This detachment, in conjunction with vitreoretinal traction, results in the accumulation of liquid vitreous fluid under the retina.
Causes of Rhegmatogenous Retinal Detachment
Risk factors include the following:
- Myopia
- Previous cataract surgery
- Ocular trauma
- Lattice retinal degeneration
Having a family history of retinal detachment
Rhegmatogenous Retinal Detachment Symptoms
- Brief flashes of light (photopsia) in the extreme peripheral vision
- Ring of floaters or hairs near the central vision’s temporal side
- Dense shadow progressing from peripheral to central vision
- Impression of a drawn veil or curtain over vision
- Straight lines (scale, edge of the wall, road, etc.) appearing suddenly curved
- Central visual loss
Rhegmatogenous Retinal Detachment Prevention
- Avoid direct and indirect injury to the eyes
- Regular eye check up
Types of Rhegmatogenous Retinal Detachment
Fresh Retinal Detachment
Long-standing retinal detachment marked by proliferative vitreo retinopathy change
- Grade A- vitreous diffuse haze and tobacco dust
- Grade B- wrinkling of inner retinal surface & reduced movement in the vitreous gel
- Grade C- rigid full-thickness retinal folds with heavy vitreous condensation and strands
Diagnosis
- Ophthalmoscopy preferably with indirect ophthalmoscope
- Fundus photography
- Ultrasound B scan
Treatment
- Retinal laser photocoagulation and cryopexy
- Scleral buckle surgery
- Pneumatic retinopexy
- Vitrectomy surgery
Based on factors such as the source and location of the lesion, the treatment approach to rhegmatogenous retinal detachment varies. These methods aim to close the retinal break via laser treatment or cryotherapy. In scleral buckling, a piece of silicone is positioned on the sclera, causing an indentation that pushes the retina inward, alleviating vitreous traction. The subretinal fluid may be drained during this process. Pneumatic retinopexy, where gas is used to reattach the retina and vitrectomy, can be a further treatment option. This is a process that involves the removal of the vitreous gel and infusion into the eye with either gas or silicone oil. The retinal injury may also be repaired by the use of laser photocoagulation with individual lasers, or cryopexy. In most cases of rhegmatogenous retinal detachment, surgery is highly effective.
When rhegmatogenous detachment is induced by vitreoretinal tension, vitrectomy is frequently used as a therapy. This growing prevalent surgery involves removing the vitreous gel and replacing it with gas (SF6 or C3F8) or silicone oil. The vitreous cavity is filled with either gas (SF6 or C3F8) or silicone oil (PDMS) after vitrectomy. A potential drawback of silicone oil is that it can cause myopia, and it must be removed within six months. Using gas, on the other hand, necessitates optimal patient positioning following surgery; the gas is absorbed within a few weeks without creating myopic changes.
Frequently Asked Questions
Certainly, if immediate treatment is not initiated, even a small reduction of vision due to partial retinal detachment may lead to complete blindness.
Individuals with retinal detachment have no possible benefits from any of the medicines, eye drops, vitamins, herbs, or dietary changes.
The success of retinal detachment surgery varies based on the seriousness of the condition and the promptness of receiving specialized medical attention. A complete recovery is possible for individuals, particularly if the macula, which plays a crucial role in clear vision and is positioned at the retina’s center, remains undamaged. Nevertheless, for those with macular damage and delayed treatment, complete restoration of vision might not be achievable.
The likelihood of retinal detachment in the other eye increases if it also has the underlying condition (like lattice degeneration) that is linked to retinal detachment in the first eye. However, if only one eye experiences a significant injury or needs eye surgery, this event does not elevate the risk of detachment in the other eye.






