Cataract Treatment in Vileparle and Santacruz
Cataract Diagnosis & Treatment
Best Retinal Detachment Surgery In India
What is Retinal Detachment?
Retinal detachment occurs when the neurosensory retina is detached from the retinal pigment epithelium beneath it.
Causes of Retinal Detachment
Factors that increase the risk include the following:
- Myopia
- Previous cataract surgery
- Ocular trauma
- Lattice retinal degeneration
- Family history with retinal detachment
- Diabetic retinopathy
In conditions such as proliferative diabetic retinopathy or sickle cell disease, vitreoretinal friction is caused by preretinal fibrous membranes resulting in tractional retinal detachment.
Conditions like profound uveitis in the case of Vogt-Koyanagi-Harada disease, choroidal hemangiomas, and primary or metastatic choroidal cancers, may make fluid leaks in the subretinal space causing Serous detachment.
Aging, trauma, or any underlying eye condition can cause a tear or hole in the retina that allows the vitreous gel to accumulate behind it, this can cause rhegmatogenous detachment.

Retinal Detachment Symptoms
The following are various symptoms that may indicate retinal detachment:
- Brief flashes of lightphotopsia in the far peripheral outer part of vision are a significant sign of retinal detachment.
- In most cases, a sudden and significant increase in the number of floaters is among the main symptoms of retinal detachment. A circle of hair-like floaters starts to be located on the side of the central vision
- The gradual progression of a curtainlike veil from the side to the central vision creates a sensation as if a curtain has been drawn over the field of vision.
- Appearance of straight lines or objects as bent or curved due to distortions in vision. The loss of central vision is another sign of retinal detachment.
Types of Retinal Detachment
Rhegmatogenous Retinal Detachment
Tractional Retinal
Detachment
What are the Risk Factors of Retinal Detachment?
Below are factors found to be causing retinal detachment:
- A past case of retinal detachment in one eye.
- History of eye surgery like cataract removal.
- Aging is also a risk factor for retinal detachment.
- Retinal detachment may also occur due to a severe eye injury.
- A history of retinal detachment in the family.
High myopia (nearsightedness) increases the risk of retinal detachment due to eyeball elongation which results in thinning, tearing, or holes in the retina.
There is a higher risk for retinal detachment in people with eye diseases and conditions such as uveitis, lattice degeneration, or retinoschisis.
Preventing Retinal Detachment
- Prevent direct and indirect injury to the eyes.
- Maintain regular eye examinations.
- Preventive actions to manage risk factors like diabetes.
An Overview of Diagnosing Detached Retina
In the field of ophthalmology, these three methods are employed to diagnose a detached retina:
- Ophthalmoscopy is done by using an indirect ophthalmoscope.
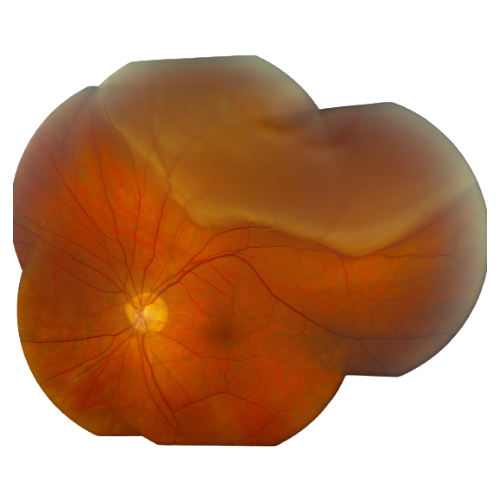
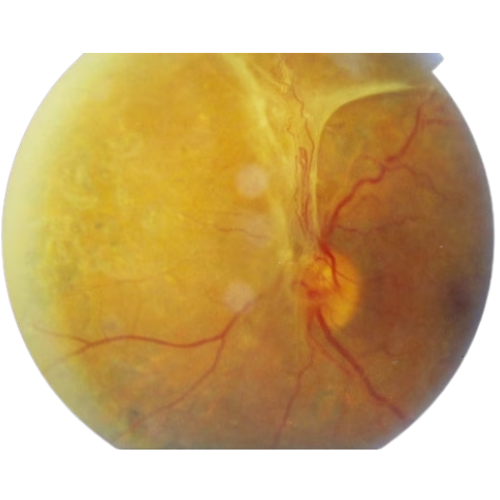
- A second method is to take photographs in the Fundus.
- It is also feasible with the use of an ultrasound B scan.
Treatment for Retinal Detachment
Below, we’ve provided an overview of various treatment options to cure Retinal Detachment:
- Retinal laser photocoagulation and cryopexy
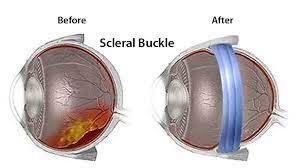
- Scleral buckle surgery
- Pneumatic retinopexy
- Vitrectomy surgery
The development and location of the lesion decide which techniques are used to treat rhegmatogenous detachment. These treatments pertain to the use of a laser or cryotherapy to seal the retinal breakage. To relieve vitreous traction, a silicone piece gets placed on the sclera, indenting it and pushing the retina inward. Fluid from the subretinal space gets drained during this treatment. Other treatment options include pneumatic retinopexy (intravitreal injection of gas) and vitrectomy. Cryopexy (freezing to scar the retinal tear) and laser photocoagulation employing green Argon, red Krypton, or Diode laser can help cure retinal breakage. The majority of rhegmatogenous retinal detachments are effectively treated surgically.
For non-rhegmatogenous retinal detachments caused through vitreoretinal traction, vitrectomy could be the preferable therapy. Systemic corticosteroids or immunosuppressive medications (e.g., methotrexate, azathioprine) are administered to treat transudative detachments.
Local therapies, such as periocular corticosteroid injections, intravitreal corticosteroid injections, or intravitreal dexamethasone implants, are another option for treating transudative detachments produced by uveitis. Primary and metastatic choroidal malignancies both necessitate therapy. Choroidal hemangiomas are treated with photodynamic treatment or, in exceptional situations, laser photocoagulation.
Frequently Asked Questions
Following retinal detachment, you should avoid doing activities such as heavy lifting, strenuous training, or postures that strain the eyes. Adherence to postoperative instructions and regular follow-ups with the ophthalmologist is essential for optimal recovery.
After retinal detachment surgery, many individuals may be able to lead normal lives. While it may be necessary to take certain precautions, progress in medical treatment has improved retinal detachment recovery and often allows for restoration of vision and functionality enabling patients to return to their usual activities with appropriate care.
A diet rich in nutrients such as omega-3 fatty acids, antioxidants A, C, and E, zinc, and lutein helps maintain retinal health. Include foods like leafy greens, fish, nuts, and colorful fruits and vegetables for their eye-protective properties. For the purpose of personalized dietary advice, it is advisable to consult a healthcare professional.
In the majority of instances, treating this eye condition requires retinal detachment surgery. It is crucial to recognize that retinal detachment is an urgent eye condition that necessitates prompt treatment.
The eye’s retina can be likened to the film found in a camera, and for a clear and precise image, it must be smooth and in good health. During the surgery, the surgeon employs various medical tools and devices to securely reposition the retina without causing any future complications.
As previously mentioned, there are several surgical options for treating retinal detachment, including scleral buckle surgery, vitrectomy surgery, and pneumatic retinopexy. Among them, pneumatic retinopexy is considered one of the simpler procedures for fixing retinal detachment. However, it may not be suitable for all cases.
In the first step of this retinal detachment surgery, the surgeon carefully injects a gas bubble in the vitreous cavity of the eye to treat the damage or the tear with cryotherapy/freezing or laser. The injected gas bubble gently presses the retina of the eye against the wall of the patient’s eye, and the freezing or the laser slowly sticks the retina down, bringing it back to its original position. Lastly, once the retinal detachment surgery is over, it is crucial to take all the preventive measures to give some time for the injected gas to gradually disappear on its own.






